Rheumatoid Arthritis
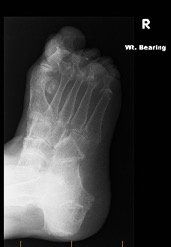
Rheumatoid arthritis is an auto-immune systemic condition that can involve multiple joints in the body. A high percentage of people with rheumatoid arthritis develop symptoms related to their foot or ankle. Symptoms normally commence in the small bones and joints of the toes and forefoot. They can then progress to the joints in the back of the foot known as the rearfoot and ankle. There are other forms of inflammatory arthritis that affect the foot and ankle including gout, ankylosing spondylitis and psoriatic arthritis. Patients with these conditions are almost always under the care of a Rheumatologist who is a specialist of joint disease.
The exact cause of rheumatoid arthritis is unknown however there are several theories including a genetic predisposition and a chemical or environmental trigger to activate the disease. As an auto-immune condition, the body’s defence system turns on itself and produces substances that attack and inflame its own joints. With 25% of the body’s total bones being located in the foot and ankle, it makes sense this condition is commonly encountered in the foot and ankle.
Rheumatoid arthritis is a complex medical condition which requires multi-modal management by a team of healthcare professionals. This involves input from the patient’s General Practitioner and Rheumatologist who may employ a combination of drug therapies to control the disease and its effects.
Addressing physical and mechanical deformities of the foot and ankle which can result from rheumatoid arthritis is paramount. This may include specialist footwear advice from a podiatrist and the use of prescription foot orthoses or braces to assist in the mechanical function of the foot and ankle. Specialised offloading techniques in these devices may also need to be used depending on the level of deformity and function.
Maintaining mobility is essential in the management of rheumatoid arthritis and other inflammatory or systemic arthridities. There are numerous physiotherapy techniques including stretching and strengthening exercises which can be used in the management strategy.
Surgical intervention is considered if non-surgical measures have been attempted and the patient’s activities of daily living are negatively affected. Surgical procedures to correct the associated deformities including bunions, hammer toes and advanced arthritis may be required.